Understanding the role of a glaucoma specialist
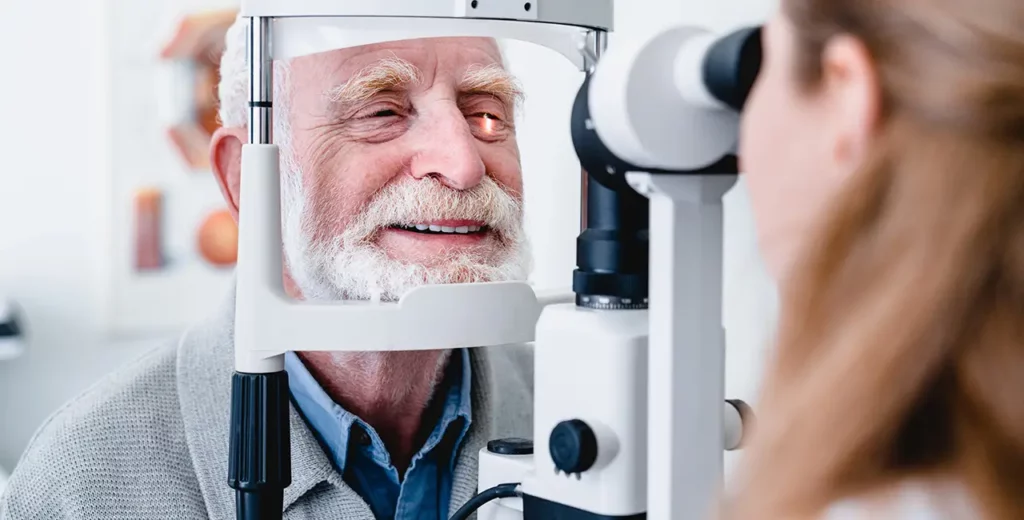
A glaucoma specialist is an eye care professional who possesses advanced training and expertise in diagnosing and managing glaucoma, a group of eye diseases that can lead to irreversible vision loss if left untreated. These specialists are often ophthalmologists who have completed additional fellowship training specifically in glaucoma. This expertise enables them to employ the most effective methods for preventing vision loss and preserving eye health.
The importance of early detection and treatment
One of the most critical aspects of managing glaucoma is early detection. Vision loss due to glaucoma is often gradual and not immediately noticeable; therefore, regular eye examinations are essential. Glaucoma specialists use various diagnostic tools to assess the optic nerve’s health and measure intraocular pressure, which is a key factor in the disease’s progression.
Early intervention can significantly slow down or even halt the progression of the disease. By identifying glaucoma in its early stages, specialists can implement a management plan that may include medications, regular monitoring, or surgical options as needed. This proactive approach not only preserves vision but also promotes a better quality of life for patients.
The role of a glaucoma specialist extends beyond just the treatment of the disease. They are pivotal in educating patients about their condition, helping them understand the significance of the disease and the importance of adhering to treatment plans. A strong patient-specialist relationship facilitates clear communication about concerns, treatment options, and lifestyle changes that may impact the progression of glaucoma.
The specialist’s approach to patient care
A glaucoma specialist adopts a comprehensive and patient-centred approach to care. This begins with a thorough evaluation of the patient’s medical history and the potential risk factors contributing to glaucoma. Specialists engage in meaningful conversations with their patients to understand their unique circumstances, which play a crucial role in tailoring individual treatment plans.
Following diagnosis, the specialist’s role includes continuous education about the condition. They empower patients to take charge of their health by providing clear, concise information about treatment options, potential side effects, and the importance of adherence to prescribed therapies. By fostering a collaborative environment, glaucoma specialists can build trust and ensure that patients feel supported throughout their management journey.
Moreover, glaucoma specialists often collaborate with other healthcare professionals to provide a holistic approach to patient care. This might involve coordinating with general practitioners, optometrists, and even dietitians to address lifestyle factors that could influence the disease’s progression. For instance, research has shown that a balanced diet rich in antioxidants can support eye health, and specialists may recommend dietary changes alongside medical treatments. Such interdisciplinary collaboration not only enhances the effectiveness of the treatment but also ensures that patients receive comprehensive care tailored to their specific needs.
In addition to clinical care, many glaucoma specialists are involved in research and advocacy efforts aimed at improving awareness and understanding of the disease. They may participate in clinical trials to explore new treatment options or contribute to educational campaigns that inform the public about the importance of regular eye examinations. This commitment to advancing the field of glaucoma care not only benefits their patients but also contributes to the broader community by fostering a greater understanding of this often-overlooked condition.
The comprehensive glaucoma assessment
When visiting a glaucoma specialist, one can expect a thorough and systematic assessment of their eye health. The comprehensive glaucoma assessment is designed to evaluate the extent of the disease and determine the most appropriate treatment strategy.
What to expect during your appointment
During your appointment with a glaucoma specialist, you will undergo several tests to assess the condition of your eyes. Initially, the specialist will take a detailed medical history and perform a visual acuity test to determine how well you see. Following this, a tonometry test will be conducted to measure the pressure inside your eyes.
Additionally, a specialist may perform a visual field test to check for any loss of peripheral vision, as glaucoma can affect side vision before central vision. Optical coherence tomography (OCT) may also be used to obtain detailed images of the optic nerve, which helps in assessing any potential damage caused by the disease. These tests are crucial as they not only provide a snapshot of your current eye health but also establish a baseline for future comparisons, allowing the specialist to monitor any changes over time. Read more about nerve on https://my.clevelandclinic.org/health/body/22584-nerves
Moreover, the assessment may include a dilated eye exam, where the specialist uses special drops to widen your pupils. This allows for a more comprehensive view of the internal structures of your eyes, including the retina and optic nerve head. The dilation process can be a bit uncomfortable, but it is vital for a complete evaluation. The specialist may also discuss your family history of eye diseases, as genetics can play a significant role in the development of glaucoma, making it essential to consider hereditary factors in your assessment.
Interpreting the results of your glaucoma tests
After the assessment, the glaucoma specialist will discuss the results with you in detail. They will explain what the tests indicate about your eye health, including the presence of any damage to the optic nerve and the level of intraocular pressure. Understanding your results is crucial, as this information forms the basis for any necessary treatment plans.
If any issues are identified, the specialist will devise a management strategy tailored to your needs. They will ensure that you understand the implications of the test results and the next steps you can take to manage your glaucoma effectively. Open dialogue during this process is essential to achieving optimal outcomes. Furthermore, the specialist may provide educational resources or recommend support groups, as connecting with others facing similar challenges can be invaluable in navigating the emotional and practical aspects of living with glaucoma. It is important to feel empowered and informed about your condition, as this can significantly enhance your overall well-being and adherence to treatment protocols.
Treatment options for glaucoma
Managing glaucoma often involves various treatment options, each designed to lower intraocular pressure and protect the optic nerve from further damage. The choice of treatment depends on the type and severity of glaucoma, as well as individual patient factors.
Medications and their role in glaucoma management
Medications are usually the first line of defence in managing glaucoma. They work by either reducing the production of fluid in the eye or increasing the drainage of fluid. Eye drops are the most common form of medication prescribed, and there are several different classes available, each with their mechanism of action.
It’s essential for patients to follow the prescribed regimen closely, as missing doses can lead to increased pressure and potential vision loss. The glaucoma specialist will schedule regular follow-ups to monitor the effectiveness of the medications and make adjustments as necessary. Additionally, patients are encouraged to maintain open communication with their healthcare providers regarding any side effects or difficulties they may encounter with their treatment, as this can significantly influence the success of the management plan. Click here to learn more about communication.
Beyond traditional medications, new advancements in pharmacotherapy are emerging, including sustained-release drug delivery systems that can provide longer-lasting effects with fewer applications. These innovations aim to improve adherence to treatment regimens, which is crucial in managing a condition that often has no symptoms until significant damage has occurred.
Surgical interventions for advanced glaucoma
For patients with advanced or uncontrolled glaucoma, surgical options may be appropriate. Surgical interventions aim to lower intraocular pressure through various methods, such as creating a new drainage pathway for fluid or implanting drainage devices.
These procedures can be very effective, but like any surgery, they carry risks and potential complications. A glaucoma specialist will carefully evaluate the patient’s situation before recommending surgery and will provide detailed information about what to expect during and after the procedure. Post-operative care is also a critical component of the surgical process, as patients may need to adhere to a strict regimen of follow-up appointments and medications to ensure the best possible outcome.
Moreover, there are various types of surgical techniques available, including trabeculectomy, which involves creating a small flap in the eye to facilitate fluid drainage, and minimally invasive glaucoma surgeries (MIGS) that aim to reduce intraocular pressure with less trauma to the eye. These options allow for a tailored approach to treatment, taking into consideration the patient’s specific type of glaucoma and overall health, which can lead to improved quality of life and preservation of vision in the long term.

The ongoing management of glaucoma
Once diagnosed, glaucoma requires lifelong management to prevent progression and preserve vision. Ongoing care involves regular monitoring and adjustments to the management plan as needed.
Regular check-ups and monitoring your condition
Regular check-ups with your glaucoma specialist are essential to monitor the health of your eyes and the effectiveness of your treatment plan. During these appointments, various tests will be re-evaluated to ensure that intraocular pressure remains within a safe range and to identify any changes in vision early …